Why Does Ozdikenosis Kill You? Causes, Risks & What You Need to Know
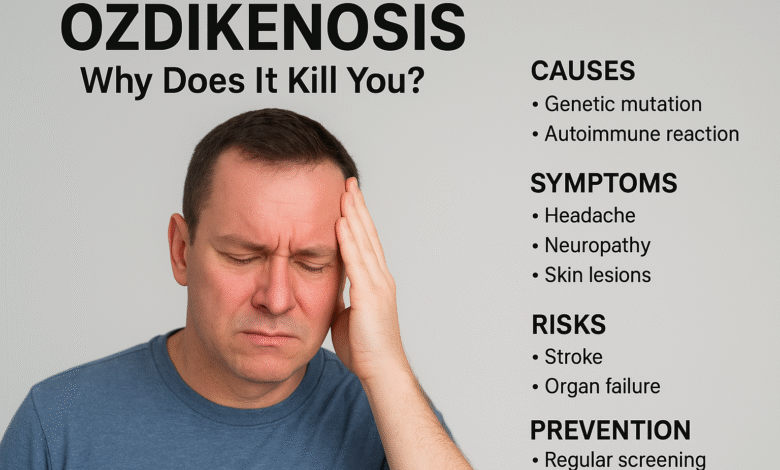
Ozdikenosis is one of the rarest and most mysterious medical conditions you may never have heard about. Its unusual name often raises a simple but urgent question: why does ozdikenosis kill you? Understanding this condition is crucial because, despite being uncommon, it poses serious threats to the body’s energy and organ function.
In this article, we will break down everything you need to know: what ozdikenosis is, why it can be fatal, the warning signs, risk factors, treatment challenges, prevention strategies, and the myths surrounding it. By the end, you will have a clear understanding of why does ozdikenosis kill you and how awareness can help manage its dangers.
What Is Ozdikenosis?
Ozdikenosis is a rare medical disorder that scientists are still trying to fully understand. Unlike common illnesses such as diabetes or heart disease, there is limited research about this condition. Simply put, ozdikenosis disrupts the way cells produce and use energy.
Cells act as tiny engines in the body, converting food and oxygen into energy. In people with ozdikenosis, these cellular engines gradually stall. This slowdown weakens organs over time and can silently progress without obvious symptoms for years. Even major hospitals acknowledge that ozdikenosis remains poorly understood, making diagnosis and treatment particularly challenging.
Why Does Ozdikenosis Kill You?
The central reason why does ozdikenosis kill you is that it impairs the body’s energy systems and compromises essential organs. Without sufficient cellular energy, vital organs such as the heart, lungs, and brain cannot function properly. When these organs fail, life becomes unsustainable.
Here’s a step-by-step explanation of how ozdikenosis can become fatal:
-
Cellular energy failure: Cells lose the ability to generate energy. Imagine a phone battery that won’t charge—no matter how much food or oxygen the body receives, the cells remain powerless.
-
Organ weakening: As cells fail, organs begin to malfunction. The heart may struggle to pump, lungs may fail to oxygenate blood effectively, and the brain may process signals poorly.
-
Immune system confusion: The immune system may attack healthy cells instead of protecting them, adding further stress to the body.
-
Gradual organ collapse: With energy depleted and immune attacks ongoing, organs fail progressively, which explains why does ozdikenosis kill you, even in individuals who appeared healthy weeks earlier.
A useful analogy is a car running with an empty fuel tank, a dead battery, and leaking oil. Initially, it may move slightly, but eventually, the vehicle breaks down completely. Ozdikenosis operates similarly inside the body.
The Science Behind Ozdikenosis
To understand why does ozdikenosis kill you, we must examine the body at a cellular level. The mitochondria are tiny organelles within cells that function like batteries, providing the energy required for movement, thinking, and overall survival. In ozdikenosis, these mitochondria fail, leaving cells powerless.
Additionally, the immune system—which normally defends against infection—can malfunction and attack healthy cells, further weakening the body.
Pros: Research has shown that mitochondrial dysfunction and immune misfires are central to the disease, giving doctors important clues.
Cons: Currently, there is no cure. Treatments can only slow progression, not stop it entirely.
Symptoms You Should Recognize
Ozdikenosis is challenging to detect early because it develops gradually. Many individuals are unaware they have it until severe symptoms appear.
Early signs:
-
Persistent fatigue
-
Muscle weakness
-
Brain fog or difficulty concentrating
Later signs:
-
Pain in organs such as the liver or kidneys
-
Heart irregularities, including fast or uneven heartbeat
-
Frequent infections due to weakened immunity
| Symptom Type | Signs |
|---|---|
| Early | Fatigue, Muscle Weakness, Brain Fog |
| Later | Organ Pain, Heart Problems, Frequent Infections |
Some symptoms remain silent, which is why ozdikenosis can be deadly before noticeable signs appear.
Who Is Most at Risk?
Not everyone has the same likelihood of developing ozdikenosis. Certain factors increase vulnerability:
-
Genetics: A family history of the disease or related mitochondrial disorders raises risk.
-
Age: Both children and adults can be affected, but adults may experience more severe effects.
-
Environmental triggers: Long-term stress, exposure to toxins, or prolonged illness can activate the disease in genetically susceptible individuals.
| Factor Type | Examples |
|---|---|
| Genetics | Family history, mitochondrial disorders |
| Age | Children vs Adults |
| Environment | Stress, toxins, long infections |
Why Treatments Don’t Fully Work
Doctors have explored various treatments for ozdikenosis, but none can fully cure it.
-
Temporary relief: Vitamins, energy supplements, or drugs like steroids may ease symptoms but do not resolve the underlying energy deficit.
-
Real-world limitations: Some treatments that work in animal models fail in humans.
-
Experimental therapies: Gene therapy and stem cell research show promise but are still in early stages.
Pros: Some patients experience improved quality of life and slower disease progression.
Cons: The disease continues to advance, and no therapy completely stops it.
The Harsh Reality
Living with ozdikenosis is difficult not only physically but emotionally and financially. Patients and caregivers often experience stress, anxiety, and social isolation. Treatment costs are high, and insurance coverage may be limited due to the rarity of the disease. Ethical concerns also arise because research is limited, leaving families to rely on experimental treatments.
Can Ozdikenosis Be Prevented?
While there is no full prevention, some strategies may reduce risks:
-
Genetic screening: Helps identify carriers and allows early planning.
-
Healthy lifestyle: Proper nutrition, good sleep, stress management, and avoidance of toxins can strengthen the body’s defenses.
Pros: May reduce flare-ups, support overall health, and help families plan ahead.
Cons: Cannot eliminate the disease entirely, and screening may be costly or inaccessible.
Myths and Misunderstandings
Because ozdikenosis is rare, misconceptions are common:
-
Myth: “It’s not real.”
-
Fact: Ozdikenosis is a genuine medical condition.
-
Myth: “It kills everyone immediately.”
-
Fact: Some patients live for years with proper care, while others deteriorate faster depending on genetics and environment.
Trusted sources such as rare disease centers and reputable medical institutions are critical for accurate information.
Living with Ozdikenosis
Though challenging, patients can improve quality of life with structured routines, healthy habits, and mental health support. Regular check-ups, stress reduction, and energy supplements may help maintain strength. Support groups and counseling reduce fear and isolation. Ongoing research offers hope for better therapies in the future.
FAQs About Ozdikenosis
1. What is ozdikenosis in simple words?
It is a rare disease that damages the body’s energy systems (mitochondria) and confuses the immune system, gradually weakening organs.
2. Can you survive it?
Yes, some people live for many years with careful management, while others progress faster depending on health, genetics, and care.
3. Why does it kill faster in some people?
Faster progression occurs when cellular energy fails more quickly or when the immune system attacks healthy cells. Stress and infections can accelerate deterioration.
4. Is it genetic or environmental?
Ozdikenosis is mostly genetic, but environmental factors like toxins and infections can worsen it.
5. Can kids get it?
Yes, children can develop ozdikenosis, with symptoms sometimes appearing later. Adults often experience more severe effects due to weaker resilience.
Conclusion
The question why does ozdikenosis kill you can be answered simply: the disease gradually shuts down cellular energy, weakens organs, and misguides the immune system. These combined effects make it life-threatening.
Although rare, awareness of symptoms, risk factors, and preventive measures can improve outcomes. Early diagnosis, lifestyle management, and ongoing research provide hope for extending life and enhancing care for those affected.



